Infants born following severe birth asphyxia are apneic and bradycardic and require immediate resuscitation, although the procedures that optimally resuscitate asphyxic infants at birth are unknown. Current resuscitation guidelines are largely based on studies in newborn animals 1-2 days after birth that have already successfully undergone the fetal to neonatal transition. However, as the physiology of an infant at birth is very different to the physiology of a newborn infant hours/days after birth, the optimal resuscitation procedures are likely to be different. Specifically, at birth, the airways are liquid-filled, pulmonary vascular resistance (PVR) is high and pulmonary blood flow (PBF) is low. As a result, gas exchange is prevented by the presence of airway liquid and as PBF is low, left ventricular output (LVO) is constrained by a lack of venous return (preload). Thus, optimal resuscitation procedures must be able to facilitate lung aeration to initiate pulmonary gas exchange and to increase PBF to initiate the transition of the cardiovascular system into a postnatal phenotype.
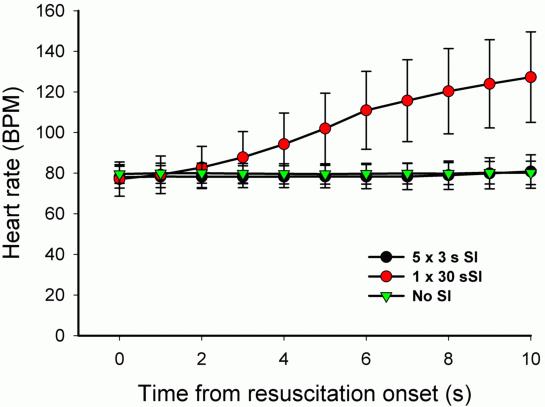
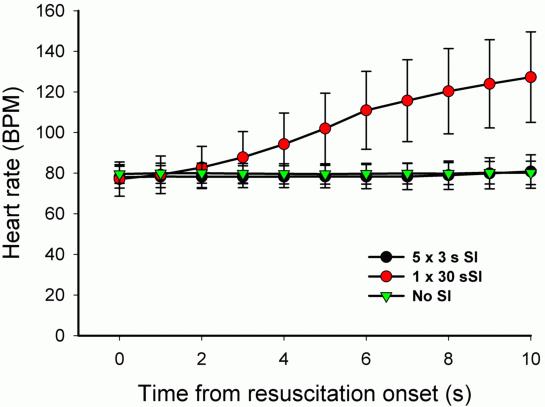
Our recent studies using phase contrast X-ray imaging have demonstrated that initiating ventilation at birth with a single 20 s sustained inflation (SI) is very effective at aerating the lung. It not only increased the rate of lung aeration and functional residual capacity (FRC) development but also markedly increased the uniformity of lung aeration. As a result, with the subsequent onset of tidal breathing, the distribution of ventilation within the lung was more uniform than if ventilation had begun using a conventional strategy. We also found that a SI accelerates the increase in PBF at birth, which is surprising because a sustained increase in airway pressures reduces PBF following lung aeration. In view of these findings, we investigated whether a single SI may optimally restore cardiorespiratory function in severely asphyxic newborn lambs at birth. A single SI of 30 s in duration was compared with conventional ventilation (60 bpm) and with five, 3 s inflations. The latter is the strategy recommended by a number of European resuscitation guidelines, although there is no evidence to support such a recommendation. The primary outcome was the return in cardiac function (heart rate, blood pressure and carotid blood flow) and respiratory function. Remarkably, a single 30 s SI, was found to trigger an increase in heart rate within 4 s of beginning the SI, which increased from 75-80 bpm to >150 bpm within 15 s, the mid way point through the SI. In contrast it took on average 74 s and 93 s for heart rates to exceed 150 bpm in lambs receiving conventional ventilation and five, 3 s inflations, respectively (Figure). Similarly, restoration of all other cardiorespiratory parameters were more rapid in the 30 s SI group.
To test whether the rapid restoration in cardiac function was mediated by an increase in oxygen, the 30 s SI was repeated with 100% nitrogen, 100% oxygen and 5% oxygen (95% nitrogen). 100% nitrogen failed to trigger an increase in heart rate, whereas 100% oxygen induced the same response as air (21% oxygen) and 5% oxygen was also similar, but the heart rate response tended to be slightly slower.
These findings indicate that resuscitation of severely asphyxic lambs at birth is most effectively achieved using a SI and that using gases that have a fraction of inspired oxygen that is greater than air is unnecessary.