Background. Glucocorticoids (GC) are commonly used for the treatment of inflammatory and autoimmune conditions but impair osteoblast function and uncarboxylated osteocalcin (ucOC) secretion which, at least in mice, leads to the development of insulin resistance (Brennan-Speranza et al., 2012). The role of osteoblast function and ucOC secretion in GC-induced insulin resistance in humans is unknown. Furthermore, acute exercise increases ucOC secretion which is associated with increased insulin sensitivity after exercise (Levinger et al., 2014), however, the effects of acute GC administration on post-exercise insulin sensitivity, ucOC secretion, and ucOC signalling in humans are unknown. The aims of this study were to investigate whether GC-induced suppression of ucOC would lead to decreased basal and post-exercise insulin sensitivity and impaired ucOC signalling in humans.
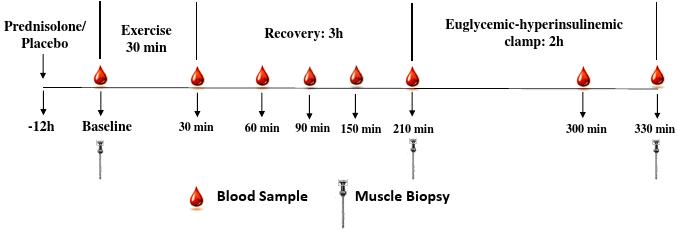
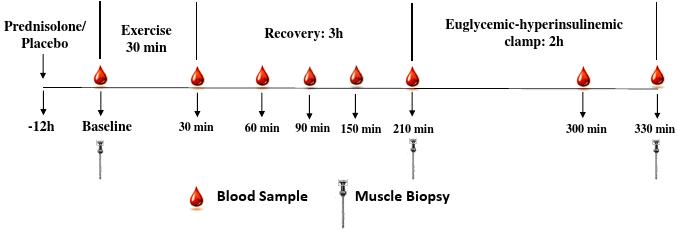
Methods. This was a double-blinded, randomized, cross-over study (refer to the Figure for an overview of the protocol). Nine healthy males (Age: 28 ± 2 years; BMI: 24 ± 1; Mean ± SEM) completed two exercise sessions, separated by 7 days, 12 hours after ingesting either GC (20 mg of prednisolone) or placebo (20 mg of Avicel). The exercise protocol included a 6-minute warm-up followed by 4 × 4-minute cycling intervals at 90 to 95% HRpeak, interspersed with 2-minute active recovery periods. The homeostatic model assessment of insulin resistance (HOMA2-IR) was used to assess basal insulin resistance and a 2-hour euglycaemic-hyperinsulinaemic clamp was commenced 3 hours after exercise to assess post-exercise insulin sensitivity (M/I Value). Venous blood samples and muscle biopsies were collected before and after exercise and insulin and glucose infusion (refer to the Figure). Serum ucOC was assessed by immunoassay and skeletal muscle protein signalling analysed via western blot.
Results. Compared with placebo, GC administration decreased serum ucOC (-24%, P < 0.01), which was associated with an increase in basal insulin resistance (HOMA2-IR: 107±27%, r = -0.54, P < 0.05) and a decrease in post-exercise insulin sensitivity (M/I value: -34±5%, r = 0.72, P < 0.01). GC administration decreased skeletal muscle protein abundance of the ucOC receptor (G protein-coupled receptor family C group 6 member A: -16%, P < 0.05), and attenuated the insulin stimulated increase in phosphorylation of glucose uptake signalling proteins mTOR Ser2481, AktSer374 and AS160Thr642 (-59%, -61% and -50%, respectively; P < 0.05). Attenuated phosphorylation of mTOR, Akt and AS160 correlated with lower serum ucOC (r = 0.61, r = 0.71 and r = 0.64, respectively; P < 0.05) and lower post-exercise insulin sensitivity (r = 0.54, r = 0.75 and r = 0.56, respectively; P < 0.05), highlighting a novel ucOC-mediated signaling pathway for GC-induced insulin resistance in humans.
Conclusions. For the first time in humans we provide evidence that GC-induced basal and post-exercise insulin resistance occurs, at least in part, through suppressed ucOC secretion and aberrant ucOC associated skeletal muscle protein signalling. Interventions targeting ucOC secretion and signalling may be a novel approach for improving glycaemic control in populations who are insulin resistant and/or undergoing GC therapy.
Brennan-Speranza TC, Henneicke H, Gasparini SJ, Blankenstein KI, Heinevetter U, Cogger VC, Svistounov D, Zhang Y, Cooney GJ, Buttgereit F, Dunstan CR, Gundberg C, Zhou H, Seibel MJ. (2012) Osteoblasts mediate the adverse effects of glucocorticoids on fuel metabolism. J Clin Invest, 122(11): 4172-4189.
Levinger I, Jerums G, Stepto NK, Parker L, Serpiello FR, McConell GK, Anderson M, Hare DL, Byrnes E, Ebeling PR, Seeman E. (2014) The effect of acute exercise on undercarboxylated osteocalcin and insulin sensitivity in obese men. J Bone Miner Res, 29(12): 2571-2576.